Osteoporosis symptoms & treatment in Chicagoland
Find an ortho specialistOsteoporosis is called a silent disease because people who have it often don’t notice symptoms.
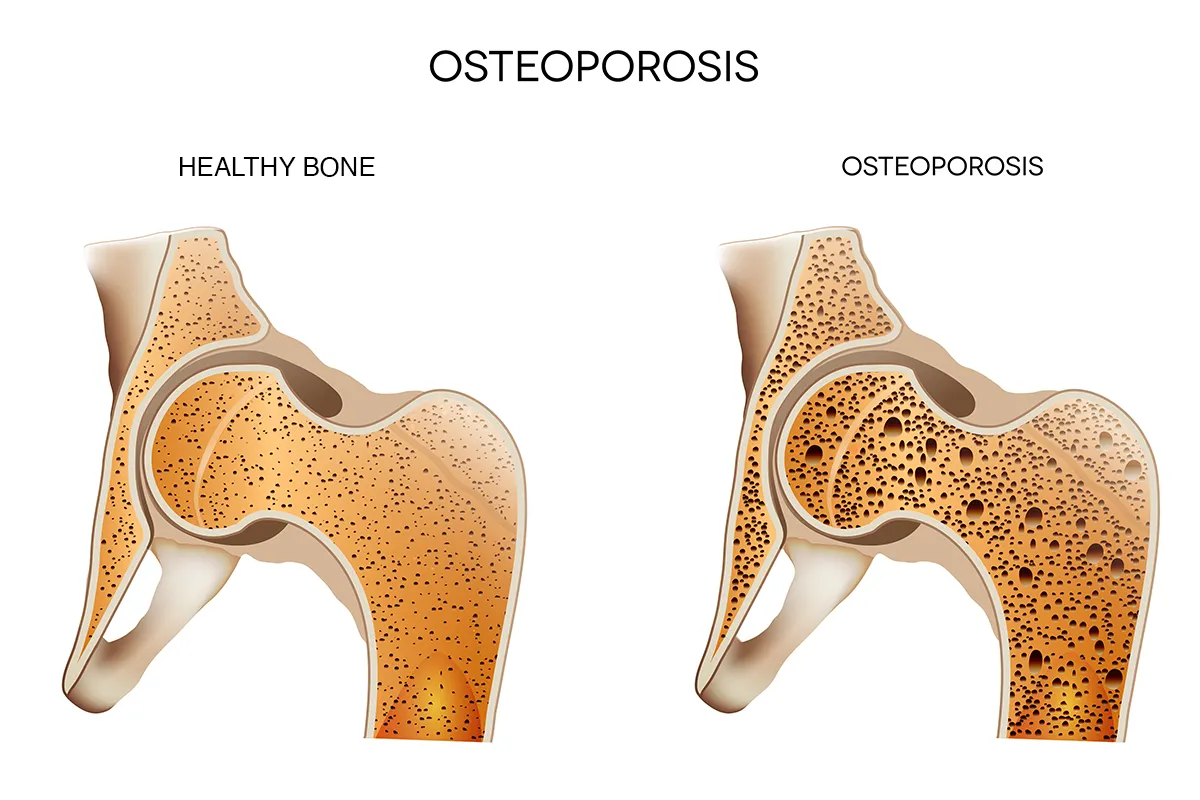
When your bones are healthy, old bone tissue is constantly replaced by new bone tissue. Osteoporosis is a bone disease in which old bone is not replaced by new bone fast enough, causing a decrease in bone mass and bone density. Over time, your bones become weak and brittle and may break easily – even from lifting light objects, bending, coughing or a minor fall.
Why choose Advocate Health Care for osteoporosis treatment?
Advocate orthopedics is proud to be ranked top 50 in the nation by U.S. News & World Report (Advocate Lutheran General Hospital) as well as top 10% in the country (Advocate Christ Medical Center, Advocate Good Shepherd Hospital, Advocate Condell Medical Center, Advocate Good Samaritan Hospital, Advocate Illinois Masonic Medical Center and Advocate Sherman Hospital).
We even received a Star Performer designation from the American Orthopaedic Association (AOA) for participation in the association’s Own the Bone program.
Schedule an orthopedic appointment
From recent injuries to nagging aches and pains, our orthopedic specialists can help. Schedule your orthopedic appointment in LiveWell, online or by phone.
Osteoporosis symptoms
Osteoporosis is a bone disease that causes progressive bone loss. Even if you have no symptoms, you may be at higher risk of broken bones.
Very early symptoms of bone loss may include:
- Receding gums or losing teeth as the jaw loses bone
- Low grip strength in hands
- Brittle fingernails
If you already have significant bone loss, signs of osteoporosis can include:
- Bones that fracture easily
- Collapsed or fractured vertebrae
- Height loss over time
- Kyphosis (a stooped or curved posture) when sitting or standing
- Back pain
The four stages of osteoporosis
Osteoporosis develops gradually – in four stages over many years – and it’s often not diagnosed until you break a bone.
Osteoporosis stage 1
Between ages 20-40, your bones break down at the same rate as new bone tissue is being made. This is considered the first stage of osteoporosis because this is the first time since birth that bone growth is no longer outpacing bone loss. There are no osteoporosis symptoms at this stage, and your bone density will be normal.
Osteoporosis stage 2
At this stage bone loss starts to outpace bone growth. If you break a bone or get bone density testing, you might be diagnosed with osteopenia, or slight bone loss. You may not have any symptoms of bone loss.
Osteoporosis stage 3
This is the stage where osteoporosis begins. You may not notice any osteoporosis symptoms, but you’ll be at increased risk for broken bones – even from simple injuries that previously would not have caused a fracture.
Osteoporosis stage 4
This is the most severe form of osteoporosis, and it’s the only stage where you may physically notice bone loss in your general appearance. Softer and weaker bones can show in the form of a bent-over appearance and pain with daily activities. Most people at this stage have had one or more bone fractures.
What are the main causes of osteoporosis?
The main cause of osteoporosis is when enough bone mass and bone density is lost that your bones become weaker and thinner. The bones most often affected by osteoporosis are the hips, wrists and vertebrae in the spine.
Many risk factors increase your chances of developing osteoporosis, including:
- Age: New bone growth slows as you age.
- Alcohol abuse: Frequent, chronic drinking.
- Diet: A diet low in calcium and vitamin D, poor protein intake, or excessive dieting for weight loss.
- Family history: When a parent has a history of osteoporosis or hip fracture.
- Gender: Women are at greater risk for osteoporosis. Men are also at risk, but they are more likely to get osteoporosis after age 70.
- Hormones: Low levels of estrogen in women and low levels of testosterone in men.
- Medical conditions: Gastrointestinal diseases, rheumatoid arthritis, endocrine and hormonal diseases, HIV/AIDS, anorexia nervosa and some cancers.
- Medications: Many medications, including some cancer medications and glucocorticoid steroids, are risk factors.
- Physical activity: Low levels of physical activity and prolonged periods of inactivity.
- Race: Osteoporosis is most common in Asian women and non-Hispanic White women and men.
- Smoking cigarettes: Studies show that smoking is a risk factor.
Osteoporosis diagnosis
It’s only after breaking a bone that some people are diagnosed with osteoporosis. Doctors also diagnose osteoporosis during routine screenings for the disease. Your doctor may recommend beginning screening at age 65 or younger if you have a high risk of osteoporosis.
When you visit your doctor, remember to report previous fractures and your family history of osteoporosis and bone fractures. Your doctor will ask you about other medical conditions and medications as well as your menstrual history, which can affect your risk for osteoporosis. Also be prepared to talk about your usual diet, exercise routine, alcohol use and smoking history.
Your doctor may do a physical exam to check your posture, balance and the way you walk, and to check for height and weight loss. Testing may include blood work, DEXA scan (Dual-energy X-ray absorptiometry) to measure bone mass and thickness, and X-ray, CT scan, or MRI to show any new or existing fractures.
Is that pain cause for concern?
Back, neck, hip or knee pain can cause severe discomfort and affect the way you live your life. Our pain quizzes evaluate your symptoms and risk factors and give you an idea of what to do next based on your results.
Osteoporosis treatment
We offer expert care to ensure you stay healthy and avoid complications and bone fractures from osteoporosis. Our team will evaluate your condition, discuss your test results and develop a personalized osteoporosis treatment plan that will help improve your mobility and minimize your osteoporosis symptoms.
Taking care of your bone health includes:
- Eating a nutritious diet rich in protein, calcium and vitamin D
- Limiting alcohol consumption
- Not smoking
- Doing weight-bearing exercises such as walking and lifting weights
Nonsurgical osteoporosis treatment
For nonsurgical osteoporosis treatment, your doctor may recommend the following to improve symptoms and avoid injuries:
- Exercise to increase strength, muscle mass, coordination and balance plus relieve any pain
- Instruction in correct body mechanics for work and daily activities to avoid excessive strain to the spine that can lead to fractures
- Physical therapy
- Education to prevent falls and avoid fractures
- Medications for pain or to treat osteoporosis
- Calcium or vitamin D supplements
- Weight loss counseling
Surgical osteoporosis treatment
For more advanced osteoporosis, additional osteoporosis treatment may also include spinal surgery. Methods may include:
- Kyphoplasty: First a balloon is inserted into the affected area to decompress your spine and allow you to regain lost height. Then your surgeon will inject a medical-grade substance called bone cement to stabilize your vertebrae.
- Spinal fusion: Two vertebrae are permanently fixed together to reduce pain, increase spinal stability and stop bone spurs from forming.
- Spinal nerve block: An anesthetic drug is injected near or directly into your spinal nerve. Spinal nerve blocks can provide pain relief and are sometimes used as a diagnostic tool to determine the source of your pain.
- Spinal stabilization: Your doctor implants rods, screws or locking plates in your spinal column. For less severe fractures, an orthotic vest or brace may be used instead.
- Vertebroplasty: Your doctor injects bone cement, which holds the bones of the spine in the proper position to reduce bone deformity and pain.
Osteoporosis complications
In advanced stages, osteoporosis can cause or occur along with several other health conditions including:
- Cervical spinal stenosis and myelopathy (cervical spondylotic myelopathy): A narrowing of the spinal canal in the neck area, which may cause your spinal cord to become compressed or damaged. Symptoms may include pain, numbness, tingling, balance problems, muscle weakness and dizziness.
- Hypocalcemic tetany: A condition where extremely low blood levels of calcium cause involuntary muscle contractions.
- Radiculopathy: Pressure on a nerve root that results in pain, weakness and numbness. Depending on the location of the nerve, you may also have difficulty controlling specific muscles.
- Spinal compression fracture: A break or rupture in the vertebrae (collapsed vertebrae). The most common sign is severe back pain.
Get care
We help you live well. And we’re here for you in person and online.