Parsonage-Turner syndrome (PTS)
Find a neuro specialistParsonage-Turner syndrome (PTS) is a rare neuromuscular disorder that can take on different forms. The most common form is the sudden onset of severe shoulder pain on one side of the body. But sometimes the pain comes on gradually. And sometimes it can affect both shoulders or other parts of the body.
Whatever your symptoms are, you can count on the experts at Advocate Health Care to identify your condition and find the best treatments for you.
What is Parsonage-Turner syndrome?
Also known as neuralgic amyotrophy, Parsonage-Turner syndrome usually starts with sudden pain in one shoulder. The pain has been described as sharp, aching, burning or stabbing. It may spread to the neck, arm and hand on the same side as the shoulder that hurts.
In the beginning of an occurrence of Parsonage-Turner syndrome, also known as the acute phase, pain may be severe and constant and may get worse in the evenings and at night.
Eventually, the constant pain from PTS becomes milder and you may have no pain while your shoulder is at rest. However, pain may return with some movements and last for a few hours before going away again.
When Parsonage-Turner syndrome persists, it becomes chronic and some people experience low-grade pain that may last for a year or more. Along with this pain, they may have weakness of the shoulder muscles that gets gradually worse.
About 75% of cases of Parsonage-Turner syndrome happen only once. When it comes back, it may involve:
- The same nerves as the initial occurrence
- Completely different nerves
- A mix of the same nerves and different nerves
Parsonage-Turner syndrome is also considered to be a type of peripheral neuropathy.
Causes of Parsonage-Turner syndrome
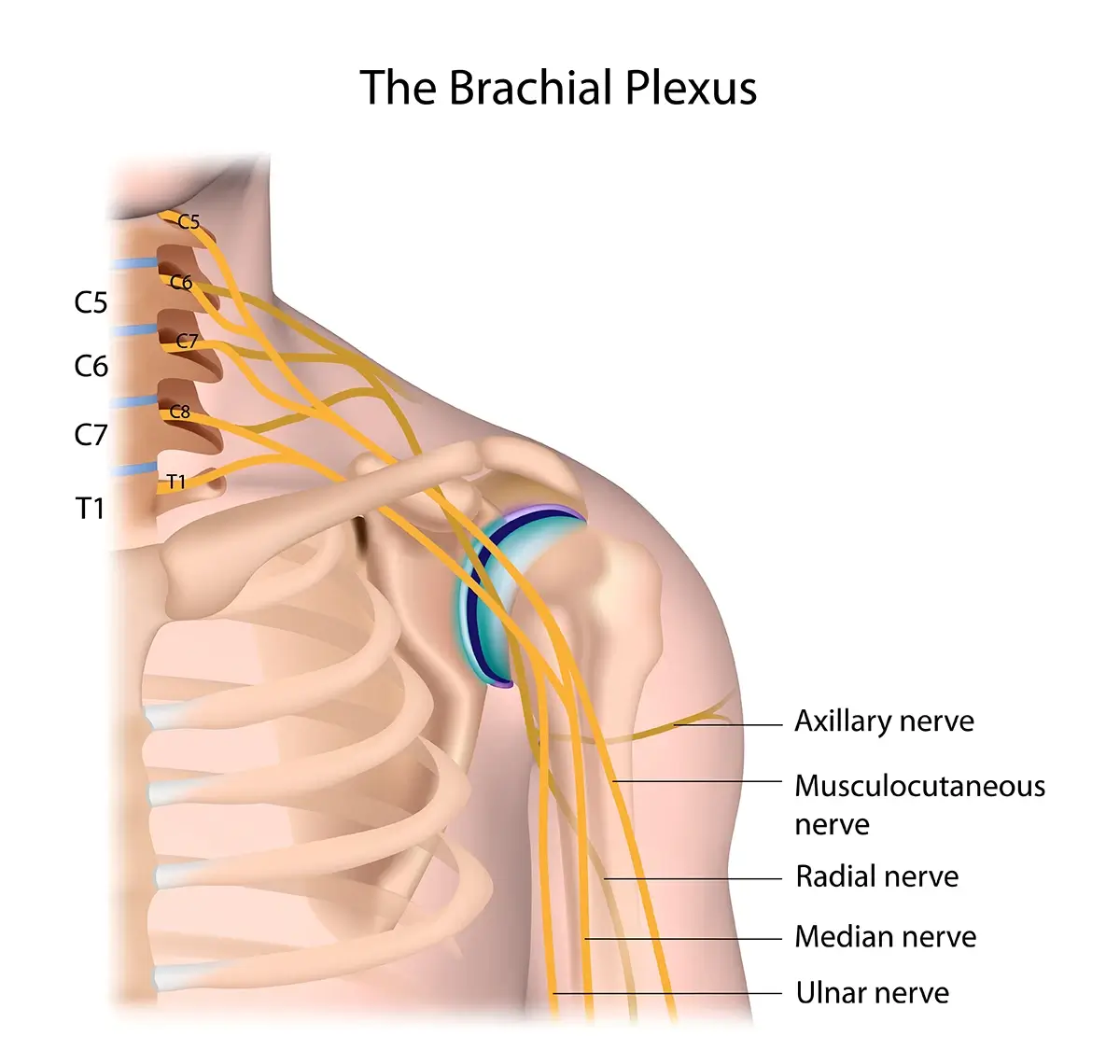
Parsonage-Turner syndrome is thought to be caused by an abnormal inflammatory response from the immune system that attacks the brachial plexus nerves, which pass through the area of the shoulder joint.
The damage to these peripheral nerves causes pain and weakness in your muscles. Improved imaging methods have revealed a characteristic hourglass-shaped constriction on nerves affected by PTS.
When nerves are damaged, they can’t send messages to your muscles well and your muscles get weaker because those messages are too weak to cause full movement. Over time, your muscles may start to shrink and become thinner (atrophy). The level of pain and weakness depends on which nerves were affected and how bad the nerve damage is.
There may be a genetic connection involved in Parsonage-Turner syndrome.
Attacks of Parsonage-Turner syndrome may be triggered by infections or other events. Having had a recent viral illness is the most common known trigger. Other possible triggers of neuralgic amyotrophy are:
- Recent vaccination
- Previous surgery on the brachial plexus
- Bacterial or parasitic infection
- Anesthesia
- Rheumatologic diseases or autoimmune disorders
- Childbirth
In some cases, no trigger can be identified.
Risk factors for Parsonage-Turner syndrome
Men are more likely to get Parsonage-Turner syndrome than women. Although people of any age can be affected, it most often occurs around the age of 40 or among young children and elderly people.
Symptoms of Parsonage-Turner syndrome
Initial Parsonage-Turner syndrome symptoms include severe pain followed by muscle weakness. Over time, you may develop some of these Parsonage-Turner syndrome symptoms:
- Absent or reduced reflexes
- Sensory deficits in affected areas
- Numbness or loss of sensation
- Unusual sensations such as tickling, prickling or burning
- Abnormally unpleasant and painful sensations after being touched lightly
- Lower back pain
- Shortness of breath because of effects on diaphragm
- Hoarseness and soft speech because of effects on laryngeal nerve
Blood vessels may be affected, causing the skin on your hands to become discolored or spotted. Sometimes hair and nails grow more quickly.
Parsonage-Turner syndrome symptoms may affect how your body responds to heat or cold. You may notice increased sweating, or your hands and forearms may feel cold.
Parsonage-Turner syndrome diagnosis
Prompt diagnosis and treatment of Parsonage-Turner syndrome help increase your chances of a full recovery. Your doctor will perform a physical exam and talk to you about your symptoms. Various kinds of specialized imaging tests may be used to confirm a Parsonage-Turner syndrome diagnosis, including electromyography (EMG), magnetic resonance neurography, MRI, ultrasound or nerve conduction studies.
Parsonage-Turner syndrome treatment
Since the cause of Parsonage-Turner syndrome is unknown, treatment for it involves treating the symptoms. Medications for pain management are important. Sometimes doctors recommend immobilization to minimize pain during the acute phase.
When the early PTS pain passes and EMG testing shows evidence of nerves starting to regenerate, physical therapy will be recommended. Physical therapy exercises help strengthen and stretch your muscles to help you regain strength and range of motion.
Occupational therapy may also be recommended to help you learn strategies for managing daily activities.
Surgery is sometimes used to repair nerve damage. Your doctor will use imaging to determine if surgery is an appropriate Parsonage-Turner syndrome treatment for you.
Get care
We help you live well. And we’re here for you in person and online.